Herd immunity. This expression was remembered in the coronavirus pandemic by Boris Johnson. In march, the prime minister of England has defined the herd immunity, colloquial term for group or collective immunity, as the main strategy of the government to deal with the pandemic as long as there was no vaccine.
This decision had generated a lot of controversy all around the world, being questioned by some – mainly the healthy scholars and healthy authorities- and copied by other state leaders, like the brasilian president, Jair Bolsonaro.
With the current stability, or even fall in some regions, of the coronavirus infections in the country, some tend to defend that the group immunity is happening here in Brazil and that maybe this strategy was accurate. But, is it really happening or is it just an illusion?
To learn a little more about this and explain better to you understand what is happening now, we’ve talked to Jamal SuleimanF infectologist from the Immunology Institute Emilio Ribas, a reference in infectious diseases and sentinel for national and international organizations; Cristina Bonorino, doctor in Immunology (UFRGS and University of Colorado), post-doctorate in autoimmunity (National Jewish Center for Immunology in Colorado) and coordinator of the UFCSPA Immunotherapy Laboratory; and Arthur Ferrari, an pathology resident doctor.
- After all, what’s group immunity?
-
According to the portal Pfarma, group immunity is defined as “a concept created by immunologists to know how many people need to be immune so that the infectious agent does not pass through that population.”
It seems simple for a fist view, but, as said doctor Arthur, it’s important to historically contextualize the term. “It was first described in 1923, but it began to be used more in the context of public health in the 70s, mainly for childhood diseases preventable by vaccine, such as Measles and Meningitis. It is a very important factor within public health to guide vaccination policies.”
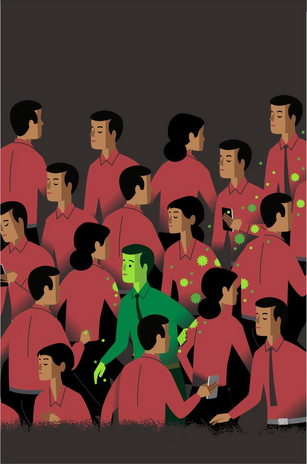
This last statement is reinforced by the fact that the group immunity is mainly used to stop the circulation of the virus by the population, through vaccination of a large percentage of it. “In fact, it happens when a particular contingent of people comes into contact with an infectious agent and produces enough antibodies to protect them. That would be herd immunity. So you have in a given environment the circulation of a certain agent with the rate of infectivity, which can vary from agent to agent and that is what will determine the time to reach that immunity. In a broad sense, when a high contingent of a given population reaches immunity against that infection.”, explains Jamal.
So, to facilitate, when the adequate percentage of the population comes into contact with the virus and becomes immune to it, even the part that didn’t have this contact is protected, because the virus will have difficulty infecting someone or even using this person as carrier, thus stopping circulating.
- Ok, understood… But, can it happen naturally, like without a vaccine?
-
There are a lot of motivations that point that it’s not possible or at least safe. The first is that it won’t affect all the people the same way and at the same time, so it wouldn’t stop the virus circulation. “It does not happen, because the natural infection, first, will happen once and it will not necessarily affect all people in the same way and if it infects a large number of people, it may be that when the immunity is in one, it will no longer be in the other. Second, this balance is dynamic, people talk a lot like that: 70% of people have the disease and in fact it doesn’t work, because people are always aging and entering in the risk group, people are traveling, people are borning, then there is not a balance due to natural infection.”, justify Cristina.
Another thing is that this policy based on natural infection is very irresponsible and would cost a lot of lives until the population gets an immunity that is not exactly guaranteed. We also need to consider if our health system would be capable of treating such a big amount of sick people. About it, doctor Arthur said that “guiding a public health policy with a context of exposing the population to contamination to achieve herd immunity is completely unfeasible, not only because we don’t know exactly how it works, but also because the health system of the country won’t be able to receive these patients.”
Also, it’s important to stand out that when we have the group immunity by vaccination, it’s easier to control how this immunity will happen and to treat the cases that have some unexpected reaction. “It is much better to use the vaccine strategy, because you control the adverse events, the adverse event is controllable, it is small and for a vaccine to be considered good, it has to have a low occurrence of adverse events, so it is much better, because you control that. It is a public health strategy to preserve the population.”, stated doctor Jamal.
- But, isn’t the falling or stabilization of the infection curve an indicative of this immunity?
-
No, it cannot be read as a signal of stabilization, because if you see the cases of other diseases, you can see that it is very common to have a fall of the cases preceded by an explosion of them, because people relax in taking the precautions indicated.
We also need to consider that this fall is not homogeneous and it’s no longer lasting, as Dr. Cristina clarifies: “If you are going to analyze, this falls have not been maintained, because they’re falls that happen in countries that haven’t controlled the pandemic (…). Here in Brazil and in the USA, nobody takes an effective providence to do it, they let it happen, so there are a lot of different curves happening at the same time. Then, when you have a fall is one of these curves, but shortly the percentages will rise again, because there is another curve rising.”.
It’s important to stand out that this fall can be linked to the knowledge we generate about the prevention of the infection and the worldwide done politics of prevention, such as the quarantine and the use of physical barriers (the masks). We need to remember that COVID-19 is a new disease and, in the beginning, we don’t have so much knowledge about how to prevent it, but it’s being constructed by practice.
“This is how it works in new diseases: in the first moment, the mortality is very high, because the care strategies are not very well defined, it’s a trial and error. (…) As the health services organize and create protocols, based on success and error, the mortality starts to fall. Today we know that, for example, it’s better to intubate someone with an altimetria less than 90% of saturation; then we can use some anti-inflammatory and anticoagulants that we didn’t know we could use. The second case is that we had the quarantine, that was made in the whole world and it’s a very effective strategy of contention”, stated Jamal.
- Ok so, in conclusion, it’s not happening in Brazil?
-
No, it’s not yet happening in Brazil. The group immunity will just happen in Brazil when we have the vaccine done and people get vaccinated. About the contingent that need to be vaccinated there isn’t a consensus yet.
“It will depend on the results of the third phase of the vaccine tests. Let’s suppose that one of these tests finds that the vaccine works and generates immunity in 60% or 70%, from that we calculate what is the percentage we need to vaccinate. As the data is too new, it is ideal to vaccinate the greatest number of people we can to protect the most fragile.”, explains doctor Cristina.
About the vaccine, there isn’t a lot of concrete information yet. In this phase of the studies, the specialists still don’t have the information of how many doses will have to be taken, whether the vaccine will have to be taken annually or if it will have mild reactions when taken.
The thing that we have to have in mind is that, when we have the vaccine it’s very important to take it, not just as an act of self preservation, but also as a gesture of empathy, because you will be protecting the health of those that are more fragile. And for those that are afraid of the adverse events, I leave here the phrase of doctor Jamal: “There is nothing in life that is not at risk. For example, I am wearing glasses, if something hit on my glasses I can have vision problems. Without glasses I can’t see, I’m at risk with it, but am I going to stop wearing glasses? No! It doesn’t make sense, because the risk of that is very low. The same case is the vaccine!”.
————————————————————————–
The article above was edited by Carolina Rodrigues.
Liked this type of content? Check Her Campus Casper Libero home page for more!